
24
Dec
Healthcare Insurance Fraud: A Persisting & Chronic Problem
Insurance fraud, waste and abuse is not a victimless act. When people cheat insurance companies out of money, insurance companies lose their financial leverage to remain operable and honest people end up paying a higher premium for insurance costs. Insurance companies lose an estimated $30 billion per year in insurance fraud costs. Excessive usage and over-utilization of healthcare manifested in various forms of insurance fraud and abuse practices makes the delicate task of balancing healthcare quality and the cost burden of care delivery while regulating access to healthcare services a daunting exercise.
Seeking Answers from Data
Our client is a leading UAE-based provider of health insurance solutions has long recognized the potential role of advanced Analytics and AI (Artificial Intelligence) in combating fraud, waste and abuse. The client has been consolidating its data analytics capabilities and needed the assistance of a trusted and competent data science partner. Cognitro worked with the client to understand early signs of fraud, detect patterns of misuse by members (and providers) and predict the likelihood of a fraud before they happen. The project was aimed at developing a new and effective approach to fraud management, one that departs from conventional tools (e.g., random auditing or whistle-blower tips) and embraces data-driven methodologies.
Putting Machine Learning to Work
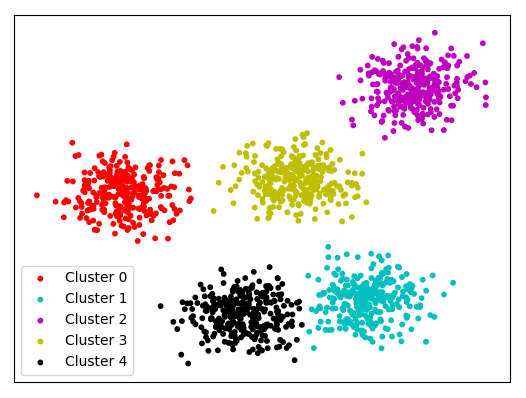
With two-year longitudinal record of members transactions spanning enrollment, doctors’ visits, hospitalization as well as claim submission, authorization and payments, Cognitro developed a predictive model that entailed two-step “unsupervised” clustering approach cascaded by a “supervised” classification model. Classic fraud detection modeling usually starts with clustering (also called segmenting) groups of users with similar behavior, and then isolating and zooming on groups that exhibit statistically unusual and alarming parameters (See figure 1).
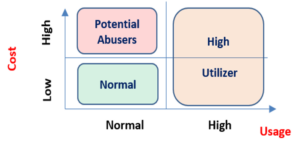
The developed clustering approach was conducted across total claim value (e.g., cost of medication, cost per visit, etc.) and frequency of usage (e.g., number of doctor’s visit, hospitalizations, emergency admissions, medication refills, etc.), and yielded a number of clusters that signified two distinct types of behaviors. First, high-utilizers or members that are relatively healthy but have a statistically abnormal pattern of frequent service usage and are incurring high cost as a result. The other is potential abusers, healthy members that have a relatively moderate level of healthcare episodes but are billing for medical services at a much higher value (See figure 2). A tree-forest classification model was then built for each cluster with the aim of scoring known/unknown members according to their propensity to fit into one of the clusters in question.
Exposing the Many Faces of Fraud
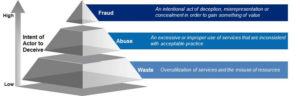
Vital analytics discoveries unveiled various patterns of suspicious behavior that vary in severity from what seems unintentional practices of overuse, cases of apparent abuse of benefits, to alarming cases of fraud (See figure 3). For example, one notable group of members with no history of chronic illnesses nor the presence of life-threatening diseases was found to have sought to obtain expensive drugs, made frequent visits to doctors, with different doctors across most visits.
Insights to Action
The direct outcome of those insights on Daman business can be realized in several ways from prompting investigation of target members, uncovering loopholes within the claim process used by fraudsters, as well as informing means to restrict and/or regulate access to certain medical services. Meanwhile, and through the success achieved in transforming its approach to combating members fraud, abuse and overutilization, the client casted all doubts about the value of is now delivering on the promise of AI and advanced analytics to optimize members and providers benefits and reshape financial, operation and medical strategy.
